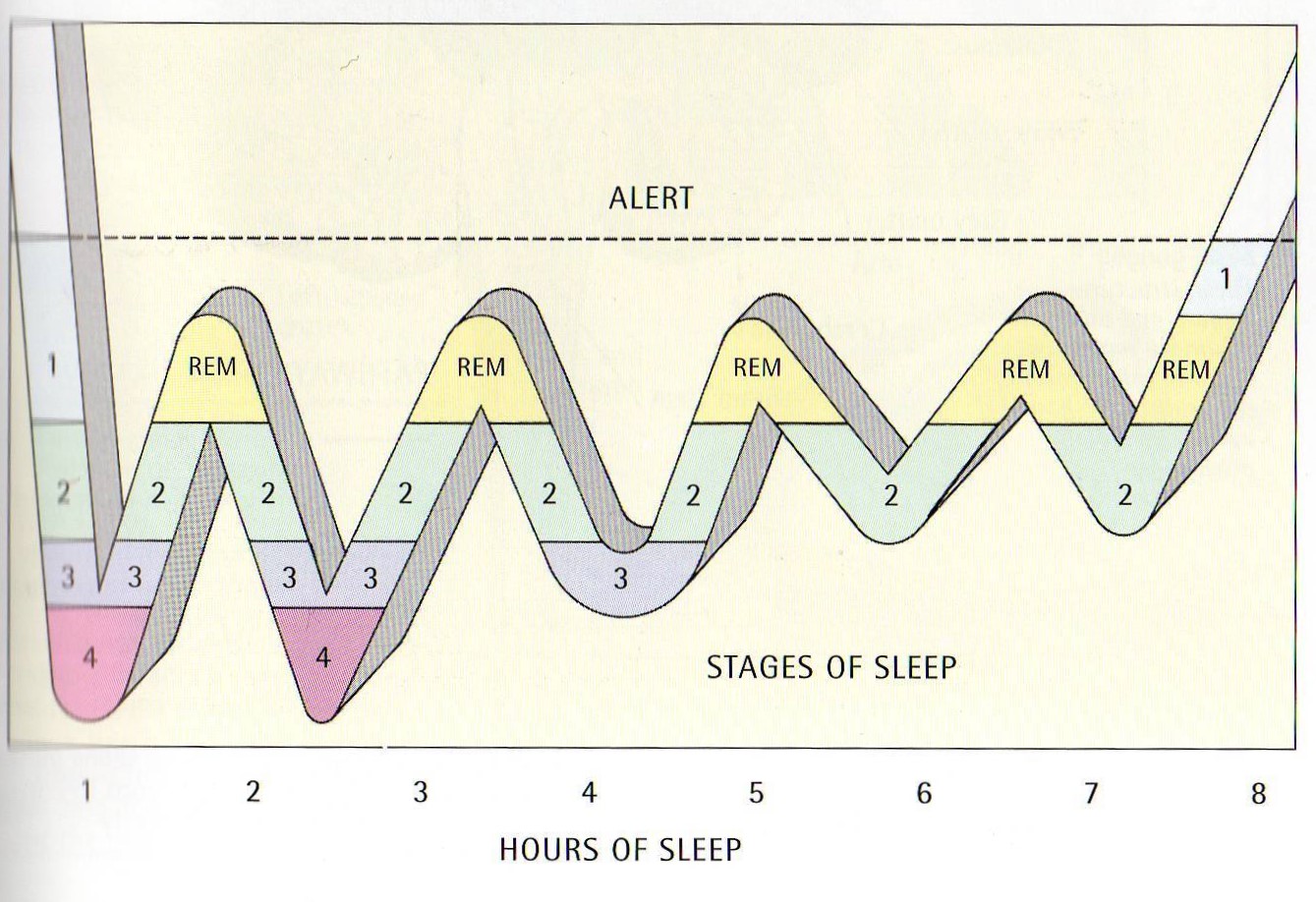
Here is the sleep cycle. It is hard-wired into our bodies. It is not an optional extra even though medications are used to tinker with it.
Our neural networks sustain these cycles using electro-chemical processes although those same processes can disrupt them. All have impact on our way to manage sleep.
Note that each cycle last between 90 – 120 minutes; you might be a 90 minuter, and I might be a 120 minute. Half of that cycle is spent sliding down into a more relaxed state. In the second half we become increasingly alert.
Over time we develop a routine that suits us but it is not difficult for it to be thrown out of kilter.
Note, also, that there are two cycles of ‘deeper’ sleep, marked 3 and 4. The brain is reasonably inactive at these time. Instead there is a great deal of bodily activity as body tissue is repaired after the wear and tear of the previous day. This is the physical recovery housekeeping stage!
There is a lot of difference between individuals.
How are these cycles disrupted?
Among other things, by sudden changes to our routines; by destabilisation of our current normal (say, by moving home, job changes, death and separations) and by high emotion. Sleep is not an optional extra. After several sleepless nights, we find ourselves dropping off during the day. We may find it more difficult to make decisions and our mood may be affected.
Some safe experiments
What follows are prescriptions and offering them goes against my best judgment, and the intended ethos of this web site. If you try out each-and-every possibility I anticipate you will get very pissed off!
So please bear in mind that any safe experiment can be effective only if it is adapted to your present lifestyle and routines. If some things in my list makes immediate sense; focus on them and only meet the others, bit by bit, if they start to make sense.
- Change routines and practise alternative habits: sleep disruption might be sorted out without going to see a doctor (that’s not a recommendation to avoid the doctor, but rather to prepare for your appointment!).
- A start can be to wake at the same time every morning, relatively early, with the help of an alarm, no matter what time you have fallen asleep the previous night. You should retire at the same time of the night without naps during the later day time or evening (NB I take a siesta after lunch quite often – a civilised continental routine – well suited to the life stage of us oldies). Siestas at tea-time, and after, are not recommended.
- Eating habits may make it difficult to get off to sleep. Eating too little may promote early waking. What is your ‘present normal’ here and what small routine might be altered?
- Smoking, alcohol and drinks containing caffeine, such as tea or coffee, can disturb sleep. They alter our state of mind. I’m not asking you to give it all up but rather to just notice your routines and their impact on you, if it is evident. Also, you can set a time to stop taking those drinks, e.g. mid- to late-afternoon).
- The same applies to any drug – legal or illegal. All drugs have side effects and some may appear to help us manage our sleep. Others positively add to our problems. Any artificial aids need to be TEMPORARY and cautiously managed by problem-solving to remove the need for artificial aids.
- We sleep badly when we are in pain or running a high temperature. That seems beyond our control, but what steps might be taken to reduce the time we are in pain or running a temperature? How do we go about alleviating these experiences?
- Talking about ordeals arising from pain, there is a safe experiment with sleep I call ‘ordeal’ therapy! What happens is that you get up from your bed after a shortish period of time of your choosing – say, 20/30 minutes of not sleeping. Find a boring and repetitive job to do such as the ironing or sorting the sock drawer. Please do not watching TV or phones as these action distort the passage of time. As soon as you feel sleepy, return to bed and return to it after the same time interval you chose. Do not assume it will happen first time around. Get up again if this does not work – until it does!
- Can other people help – for the sake of asking for things from them? For instance, if you are in a couple your time of retiring and your time for getting up may well vary, and vary a lot. Find ways to ‘allow’ for that. This strategy is trickier – easier when you are older – but ……
When a lack of sleep continues, everyday life can become trying. Anxiety can build up and we may find it very difficult to get off to sleep. It is possible to find myself in crisis, say, through a depressed state promoted by waking early, or in the middle of the night. At this time we may well need to consult our family doctor. In the 21st century there are tablets available to help us with discomfort and unsettled sleep. That’s the first aid.
For my part, I will examine further the problem-solving safe experiments rather than the ‘first-aid’ route. Further information from the NHS is available. Does it match what I am saying? It does not always work that way!
Further safe experiments – repetition deliberate!!
- Consider how you might collect some information (safe experiments need results!). When you examine your sleep routine consider the specifics. WHEN, WHERE or WITH WHOM do you prepare for sleep and get ready for it? A diary covering the mid-evening and onward – kept for a given period of time, say, one month – can help to identify these things.
- Take moderate amounts of exercise during the day-time, such as swimming or walking (not in the mid- to late evening).
- Cut down or stop drinking tea or coffee in the evening. Try a milky drink before going to bed, if it helps.
- Don’t drink alcohol. It may help you fall asleep, but will almost certainly make you wake up through the night, if only to go to the loo. Alcohol is a depressant, and attracts all the symptoms of depression.
- Don’t eat late at night, although this is tricky when you are hungry. Feeling hungry can keep us awake. Try to have your evening meal early rather than late.
- Explore ways to relax before going to bed. Some people use relaxation systems. There are many to be found on the Web. However, beware under-estimating your own ability to create your own safe place in your own head. Have a go and roam around in it.
- Make sure that your bed and bedroom are comfortable – not too hot, not too cold or too noisy.
- Listening to quiet music might help as long as any switch off does not wake you again!
- Establish a regular pattern of going to sleep and waking up at the same time every day. If necessary, restrict your sleep; go late and wake early.
- If you’ve had a bad night, resist the temptation to sleep the next day – it will make it harder to go to sleep the following night.
- If something is troubling you then write it down before you go to bed. If necessary, keep a note-pad next to your bed. This will provide a reminder or To Do list for tomorrow’s action. It is possible that some issues will appear less problematic in the cold light of day.
- If you can’t sleep, say, after 20/30 minutes, then get up and do something you find relaxing. Reading and watching television might be tempting but it is easy to lose track of time here. Instead, can you find a boring routine task you have neglected for some time; clean out the sock drawer? The key here is that the body needs to know that bed is for sleep only (and the other obvious thing!).
- After a while, say, around 20/30 minutes go back to bed again – whether you feel tired or not. Note the length of a half-cycle in the diagram above is around 45 – 60 minutes so the 30 minutes, above, is not a random or magic figure; it is not quite a half-cycle. The key here is to see if your body can tell you whether you are at the bottom or top of a sleep cycle.
- When you return to bed, and if sleep does not come quickly, use thinking-about-breathing I have mentioned before. Slow your breathing – in only through the nose – and countdown, one by one, from 1000 on the out-breath. You may find you forget the number – that is not important. Just keep counting down as best possible. The important thing here is the rhythm you are creating.
- The breathing and countdown may be quite demanding – requiring concentration – so just keep counting down slowly. This is one safe experiment that is intended to fail. If you are good with figures, and you want to make the experiment trickier, then do a countdown in threes; that is, 1000, 1997, 1994 etc.
- Let me end with a cunning strategy. If you return to bed and find you do not sleep yet again. Use slowed breathing to go back into visualisation of a relaxing scene and then use the thought that says: “I am not going to sleep, I am not going to sleep etc”.
- If your adaptations of these approaches seem not to help then talk over things with a very trusted friend or professional. Some people tell me that speaking things out seems to help devise further action required, if it is needed.
Some useful books
Get a Better Night Sleep Ian Oswald and Kirstine Adam, Optima
Why We Sleep James Home, Oxford University Press
Sleep like a Dream the Drug-Free Way Rosemary Nichol, Sheldon Press
… and the inevitable app! See: https://www.bettersleep.com/
What works for you? Do let me know.
Some leads to follow
How to design safe experiments
Evolution of the human as just one mammal
An index of pages on Your Nudge